Polycistic Ovary Syndrome
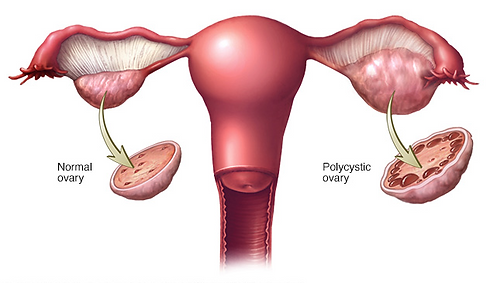
PCOS is a condition found in women who typically don’t ovulate, characterized by excessive production of androgens (male sex hormones) and the presence of cysts in the ovaries. Follicles go through the normal maturation process but fail to become eggs due to the hormonal imbalance. PCOS can range from mild to serious, and so can the symptoms. Some of the symptoms might include: excessive weight gain, acne, diabetes and excessive hair growth.
Women with PCOS have a hormonal imbalance and metabolism problems that may affect their overall health and appearance. PCOS is also a common and treatable cause of infertility.
The exact cause of PCOS is not known. Most experts think that several factors, including genetics, play a role:
-
High levels of androgens. Higher than normal androgen levels in women can prevent the ovaries from releasing an egg (ovulation) during each menstrual cycle, and can cause extra hair growth and acne.
-
High levels of insulin. Insulin is a hormone that controls how the food you eat is changed into energy. Insulin resistance is when the body's cells do not respond normally to insulin. As a result, your insulin blood levels become higher than normal. Many women with PCOS have insulin resistance, especially those who are overweight or obese, have unhealthy eating habits, do not get enough physical activity, and have a family history of diabetes (usually type 2 diabetes).
PCOS Fertility Tests
17-OH progesterone:
A blood test is used to identify why an adult female may be infertile or have excess hair growth (hirsuitism). Deficiencies may increase androgen levels leading to masculine characteristics and interfering with ovulation. Many women with PCOS have exaggerated ovarian 17-OH progesterone secretion. It can also be used to identify possible disorders in the adrenal gland such as Congenital Adrenal Hyperplasia (a group of inherited disorders associated with abnormal metabolism of adrenal gland hormones).
Androstenedione (ASD):
Measurement of ASD provides a useful tool for androgen (male hormones) biosynthesis. Elevated ASD levels have been demonstrated in congenital (a medical condition present at birth) adrenal hyperplasia (CAH – the enlargement of the adrenal glands). They are also increased in polycystic ovary syndrome (PCOS), ovarian stromal hyperthecosis, 3ß-hydroxysteroid dehydrogenase deficiency, and other causes of hirsutism (excessive facial or body hair) in women. Levels are normal in idiopathic hirsutism. Male hormones produced by the adrenal gland (called androgens) which, when found in excess, may lead to fertility problems in both men and women. Excess androgens in the woman may lead to the formation of male secondary sex characteristics and the suppression of LH and FSH production by the pituitary gland. Elevated levels of androgens may be found in women with polycystic ovaries, or with a tumor in the pituitary gland, adrenal gland, or ovary. May also be associated with excess prolactin levels.
Comprehensive Metabolic Panel (CMP):
A blood test that evaluates organ function and checks for conditions such as diabetes, liver disease and kidney disease. Specific items measured include: blood sugar level, electrolyte and fluid balance, kidney function, and liver function. Abnormal results, and especially combinations of abnormal results, can indicate a problem that needs to be addressed.
DHEA-S (Dehydroepiandrosterone sulfate, DHEA-SO 4 ):
Measurement of DHEAS, an adrenal steroid, is important to investigations of abnormal hair growth (hirsutism) in women. DHEA sulfate is performed in conjunction with free testosterone as an initial screen for hyperandrogenism (elevated levels of male hormones) in hirsutism. At least one of these two hormones is likely to be elevated in the great majority of cases. Sometimes DHEA-SO 4 is the only hormone circulating at a level above normal, and is more likely to be elevated during the early stages of hirsutism than most other androgens. High DHEA-SO 4 levels are often encountered in PCOS (Polycystic Ovarian Syndrome), showing that adrenal hyperandrogenism is a fairly typical part of this syndrome. Male hormones produced by the adrenal gland (called androgens) which, when found in excess, may lead to fertility problems in both men and women. Excess androgens in women may lead to the formation of male secondary sex characteristics and the suppression of LH and FSH production by the pituitary gland. Elevated levels of androgens may be found in women with polycystic ovaries, or with a tumor in the pituitary gland, adrenal gland, or ovary. There also may be association with excess prolactin levels.
Estradiol:
A hormone produced in the ovaries by cells that surround a developing egg (follicle). In terms of ovarian reserve, this test is used to confirm the results of a day 3 FSH. A high estradiol level may artificially lower (or mask) what otherwise would be a higher (potentially abnormal) FSH. The other two uses of this test are: 1.) for the diagnosis of amenorrhea (the absence of a menstrual period) and 2.) to monitor progress during ovulation induction.
Fasting Glucose:
Used to identify patients with either normal glucose, impaired fasting glucose (IFG), impaired glucose tolerance (IGT) or if they are suspected of having diabetes. Glucose levels in the normal ranges indicates insulin resistance with high insulin levels. Moderately high glucose levels indicate Impaired Glucose Tolerance (IGT). Very high glucose levels indicates type 2 diabetes Women with PCOS have a much higher risk of developing diabetes than non-PCOS women.
Fasting Insulin:
Insulin is a hormone that helps the body use and control the amount of glucose in blood Normally, blood glucose levels increase slightly after consuming carbohydrates. This increase causes the pancreas to release insulin so that blood glucose levels do not get too high. However, some women with PCOS tend to have chronically high levels of insulin that do not drop back to normal levels (hyperinsulism). Fasting insulin measures insulin between meals, when it should be at its lowest and is used to determine if a patient is insulin resistant. This test is done in conjunction with glucose testing to evaluate a patient’s metabolic status. Insulin resistance is thought to be one of the main causes of PCOS (Polycystic Ovarian Syndrome).
Follicle Stimulating Hormone (FSH-female):
A hormone produced by the pituitary gland that is located in the brain. It plays a key role in the development of follicles (immature eggs) into mature eggs. FSH also plays an important role in telling the ovaries when it is time to release a mature egg (ovulation). A normal FSH level indicates a woman has a good supply of eggs (ovarian reserve) and is a good candidate for ovarian stimulation in IVF. As a woman gets older and the number of eggs she has remaining becomes low it takes more FSH to produce an egg. Therefore a high FSH score indicates a low or declining egg supply (ovarian reserve). FSH values can fluctuate from one cycle to the next, so when looking at multiple FSH values the highest value is the one that is considered to be the most accurate. For example if a woman had an initial FSH of 9 and had another FSH a month later with an FSH of 5 it does not mean her ovarian reserve had improved. Her true score is still considered to be an FSH of 9.
Glucose Tolerance:
Done to check the body’s ability to process sugar. The test begins with blood being drawn in the morning after fasting overnight. The patient then consumes a special drink prepared with 75 grams of glucose (sugar). Blood is then drawn at various intervals over a period of several hours. An abnormal result in PCOS women may suggest the presence of diabetes or a pre-diabetic condition. Abnormal findings may also indicate other problems such as reactive hypoglycemia.
Hemoglobin A1c:
Red blood cells in the body contain a protein responsible for carrying oxygen called Hemoglobin. Glucose attaches to Hemoglobin to form a compound called “Hemoglobin A1C” or Glycosylated Hemoglobin. Red blood cells have a life span of about 3 months. At the end of their life span, the red blood cells are destroyed and new ones made. As a result, the amount of Hemoglobin A1C in the red blood cell is an indicator of your average blood sugar over the past 3 months giving a long-term, big picture look at blood sugar levels.
High Sensitivity C Reactive Protein (hs-CRP):
Most often used to help predict a healthy person’s risk of cardiovascular disease. The higher the value, the greater the risk of cardiovascular disease and vice versa. hs- CRP may differentiate between those PCOS women who are at higher risk of developing type II diabetes and CVD.
LH (Luteinizing Hormone, lutropin – female):
Serum LH determinations have been very useful in the diagnosis and treatment of infertility in women. A midcycle rise is a good indication that ovulation will occur approximately 24 hours later. Subfertile couples, and women being treated with gonadotropin for infertility, can be informed that ovulation is imminent. In the woman LH is necessary for the production of estrogen. When estrogen reaches a critical peak, the pituitary releases a surge of LH (the LH spike), which releases the egg from the follicle.
Lipid Panel:
A check of cholesterol types (examples include HDL, LDL) and triglycerides to assess cardiovascular risk, particularly among women who are obese. Women with PCOS frequently have high cholesterol and triglycerides. Consequently these women also have an increased risk for cardiovascular disease.
Prolactin:
A hormone that stimulates the production of milk in breastfeeding women. Increased prolactin levels in women not breastfeeding may interfere with ovulation and fertility. Prolactin has become an important tool in the investigation of amenorrhea (absence of menstruation), galactorrhea (abnormal milk production at times other than when nursing) and hypothalamic-pituitary disorders. Prolactin is a stress hormone, surgery; venipuncture, an interview, etc. may cause a transient rise.
Sex Hormone Binding Globulin (SHBG):
This protein is responsible for binding the majority of testosterone in the blood into a specific complex. Low levels of SHBG indicate insulin resistance and provides an explanation for elevated levels of Free Testosterone. Symptoms associated with hyperandrogenism such as PCOS (Polycystic Ovarian Syndrome) may be due to decreased levels of SHBG.
Testosterone:
(Total) indicates the degree of hyperandrogenism (over production of male hormones) in women. Mild to moderately high levels are associated with conditions such as: PCOS (Polycystic Ovarian Syndrome), HAIRAN, or adrenal hyperplasia. Persistently high levels of total testosterone indicate androgen-producing tumors in the ovaries. (Free) elevation of testosterone levels is a sign of hyperandrogenism (over production of male hormones). It causes an increase in luteinizing hormone (LH) that leads to an increase in the ratio of LH to FSH. An elevated LH:FSH ratio results in major changes to a woman’s cycle and fertility functions.
TSH (Thyroid Stimulating Hormone):
Stimulates the thyroid gland to produce T4 and T3. Measurement of TSH is used primarily to determine the cause of hypothyroidism (too little thyroid production). In primary hypothyroidism, the TSH level is elevated due to impaired production of thyroid hormones. In secondary or tertiary hyperthyroidism, thyroid hormone production is low due to pituitary or hypothalamic lesions. In hyperthyroidism (too much thyroid production), the TSH level is typically suppressed to subnormal levels. TSH can also be used to help determine if a patient has adequate levels of T4.


